Starting in October 2019, skilled nursing facilities (SNFs) will start receiving Medicare reimbursement payments under the Patient-Driven Payment Model (PDPM). This is the largest Medicare Part A reimbursement change since the implementation of the per diem prospective payment system (PPS) in 1998. This new case-mix payment model focuses on resident clinical characteristics rather than volume-based services provided to determine the Medicare payment.
RKL’s Senior Living clinical consultants have been working with SNFs throughout the nation to help them understand the reimbursement changes confronting the profession. Below, we’ve rounded up key information on the reimbursement model switch and offer action items to support SNFs as they adapt to the most significant change in more than two decades.
Reasons for Medicare Reimbursement Model Change
The Centers for Medicare & Medicaid Services (CMS) decision to switch from the current case-mix model (Resource Utilization Groups, Version IV, or RUG-IV) to PDPM was fueled by a number of issues, most notably a reimbursement schedule based on the amount of therapy provided to a patient regardless of unique characteristics, needs or goals.
CMS set out to redesign a model that advanced SNFs toward distinct goals:
- Elimination of financial incentives related to therapy provision
- Improved accounting for resident characteristics and care needs
- Reduction of systemic and administrative complexity
- Better alignment between resident care decisions and actual care needs
As visually represented below, the current RUG-IV model reduces everything about a patient to a single, typically volume-driven, case-mix group, PDPM focuses on the unique, individualized needs, characteristics and goals of each patient.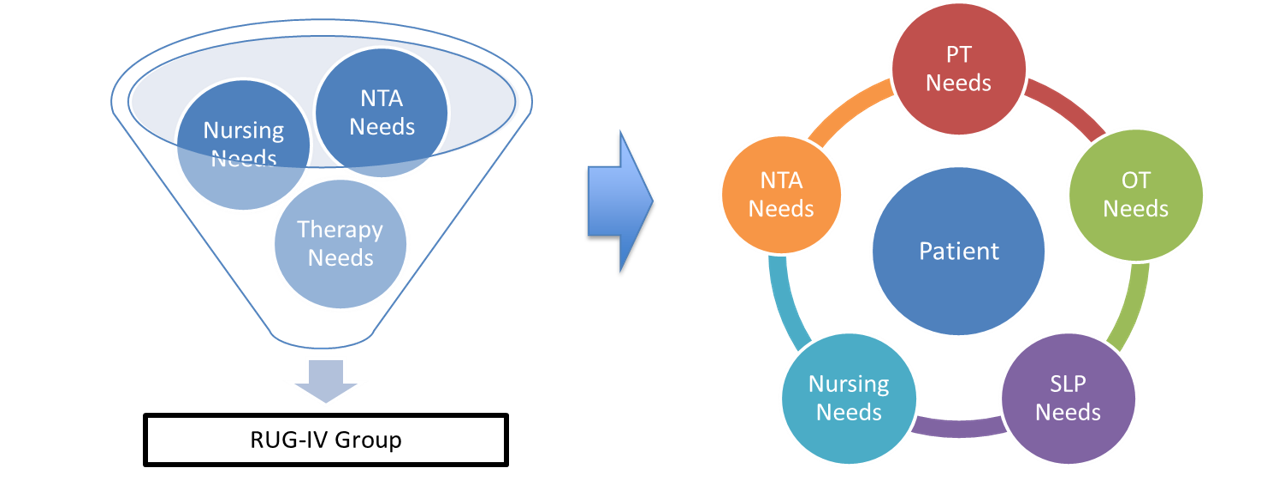
By addressing each individual patient’s unique needs independently, as demonstrated below, PDPM improves payment accuracy and encourages a more patient-driven care model.
Components and Patient Classification
To achieve the goals listed above, PDPM will provide a per diem payment based on six components, five of which are case-mix adjusted and determined by patient characteristics. PDPM goes beyond the two components of the current RUG-IV model (therapy and nursing) to include Physical Therapy, Occupational Therapy, Speech Language Therapy, Non-Therapy Ancillary and Nursing. The sixth non-case-mix component that is fixed based on facility specifics. Patients are classified into a group for each of the case-mix components listed above and scored according to a specific set of criteria for each component.
Determining Medicare Payment Rate under PDPM
Under PDPM, the per diem rate for each of the five case-mix components and the non-case-mix component is tallied. CMS will make adjustments to the Physical Therapy, Occupational Therapy and Non-Therapy Ancillary components over a stay to capture changes in resource utilization. CMS research shows that these three components account for changes to the rates over time and during the stay.
How and When to Change from RUG-IV to PDPM
Since running both systems at the same time is not feasible for providers and CMS, there will be no transition period between the current and future systems. RUG-IV billing will end September 30, 2019, and PDPM billing will start October 1, 2019.
Under the changeover to PDPM, all providers must complete a new Interim Payment Assessment (IPA) no later than October 7, 2019, for all of their Medicare Part A patients. This new IPA is required to receive a PDPM HIPPS code for use in billing starting on October 1, 2019. Keep in mind, under PDPM, October 1, 2019, will be considered Day 1 of the variable per diem schedule, even if the patient began their stay before that date. Failure to complete IPAs before the October 7, 2019, deadline are subject to late assessment penalties.
PDPM Preparation Tips
The impact of the change to PDPM cannot be understated. SNFs should prepare as early as possible and gain a thorough understanding of how this will impact their clinical operations and billing procedures. Here is a quick reminder of action items to prepare for PDPM:
- Determine the appropriate admitting diagnosis code
- Communicate with your electronic health records provider
- Shore up nursing documentation skills
- Evaluate and update processes prior to PDPM implementation
- Conduct a budget analysis
This post is a high-level overview of the major reimbursement changes under PDPM. Beyond the case-mix refinements, there are a number of other SNF policies that take effect, including revised Health Insurance Prospective Payment System (HIPPS) coding, changes to the Medicare Minimum Data Set (MDS), concurrent and group therapy limits, interrupted stay policy and more. To discuss the entire impact of PDPM within the context of your SNF’s unique circumstances, contact me.





